
-
Efficiency of Open Bite Treatment Using a Combination of 3M™ Incognito™ Appliance System and 3M™ Clarity™ Advanced Ceramic Brackets for Patient Suffering from Obstructive Sleep Apnea
Dr. Obach-Dejean, DDSExtraoral photos before treatment.

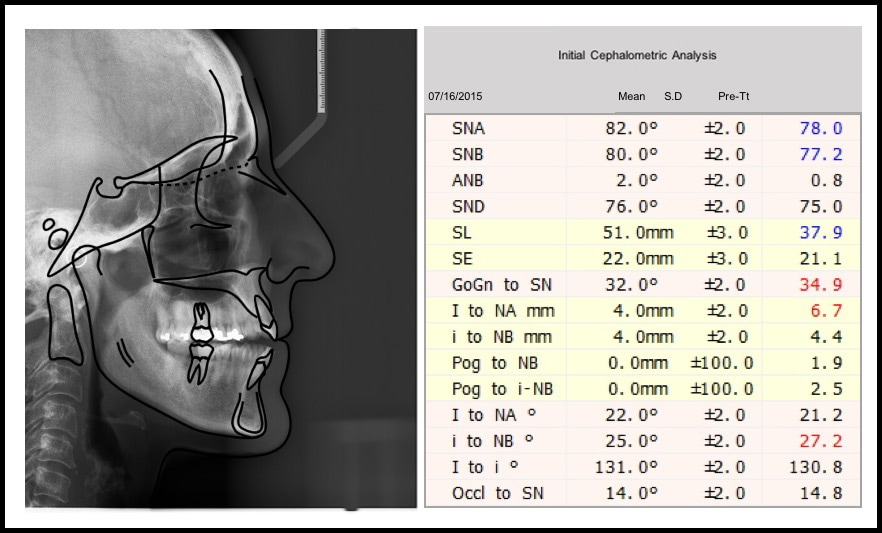
Initial cephalometric analysis.
Intraoral photos before treatment.

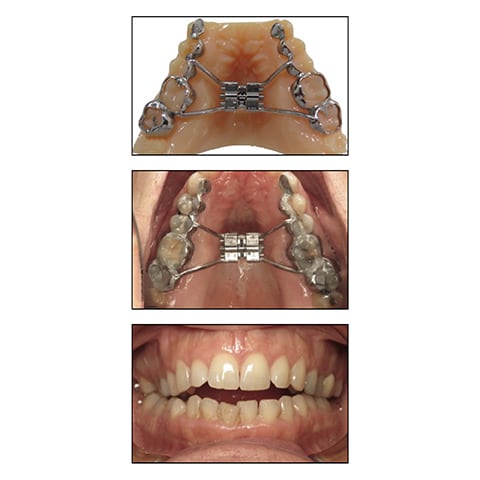
Before surgically assisted expansion.
.018x.025 Niti archwire.

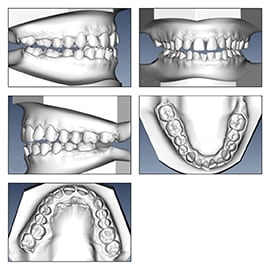
Malocclusion models.
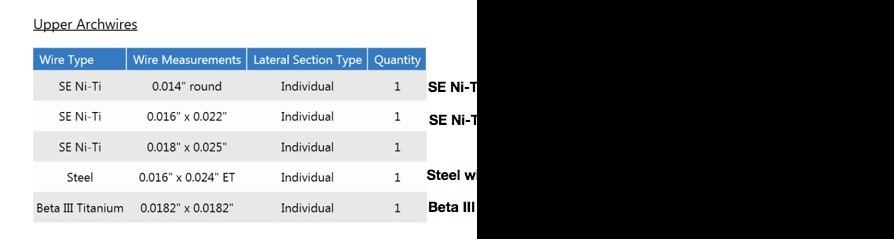
Upper archwires.
Phase II intraoral photos.

.0182x.0182 Beta 3 titanium archwire.

Maxillary retainer.

Extraoral photos at retention.

Phase II panoramic radiograph.

Intraoral photos at retention.

Panoramic radiograph before treatment.

Panoramic radiograph at retention.

0.14 Niti archwire.

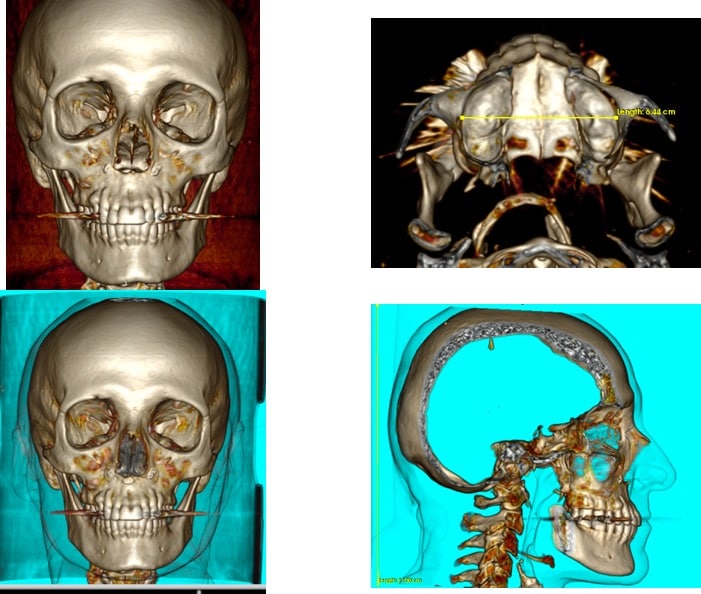
CBCT images.
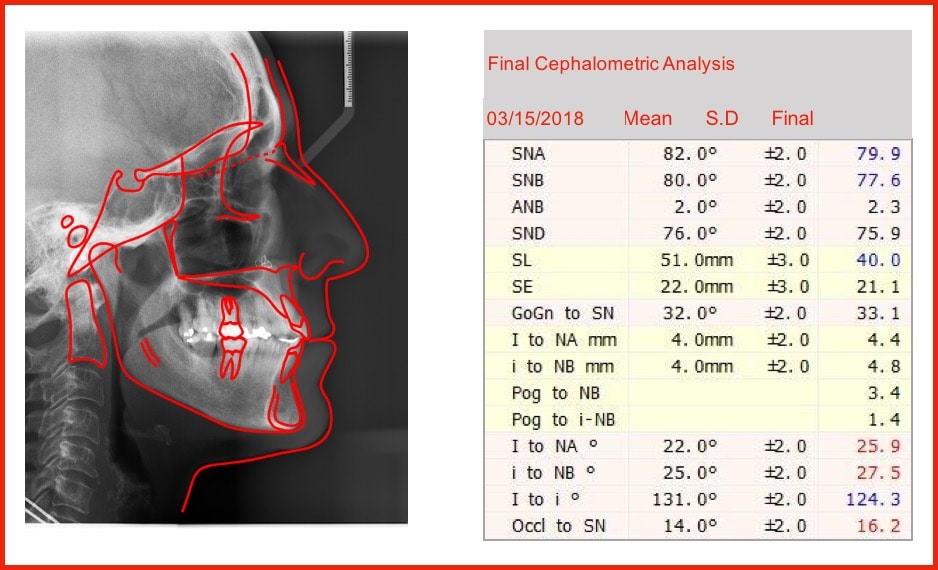
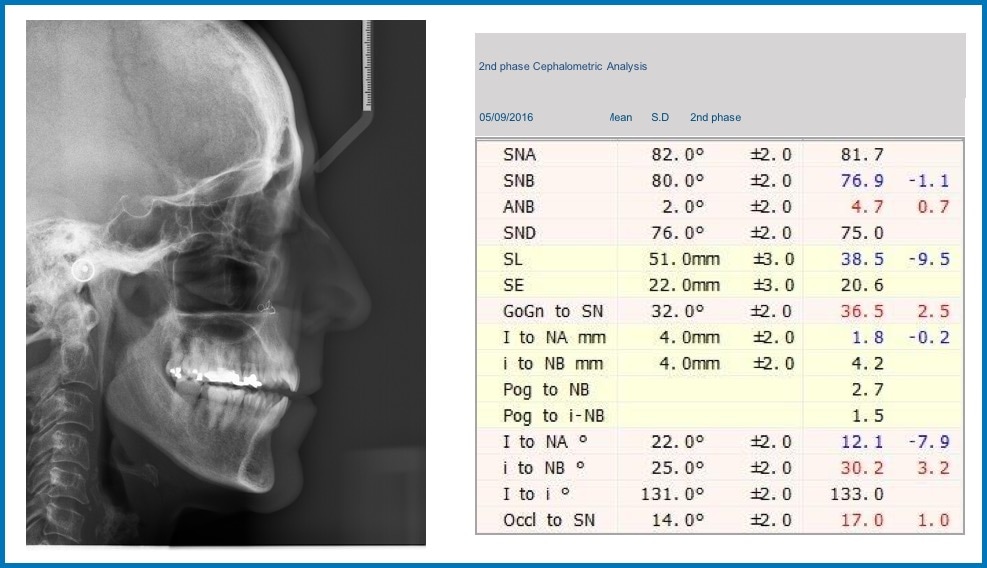
Second phase cephalometric analysis.
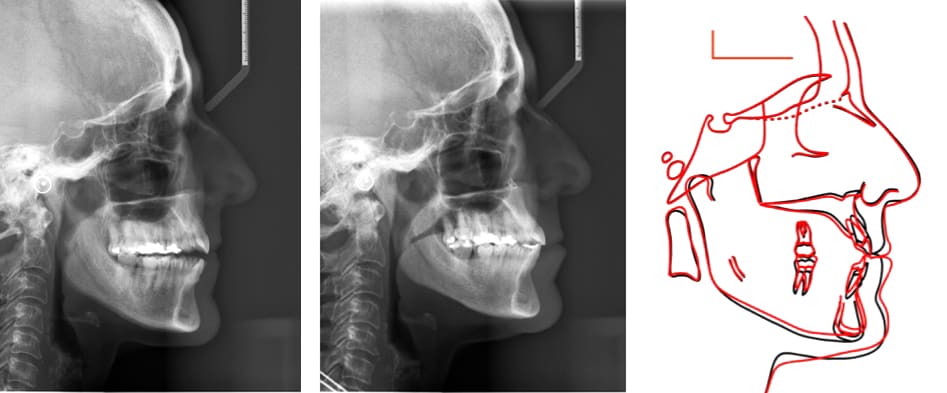
General structural superimposition.
.016x.025 Niti archwire.

CBCT images.
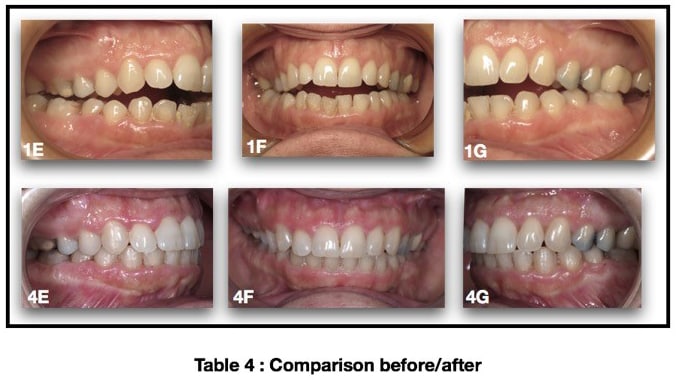
Intraoral comparison photos before and after treatment.
-
Introduction
Patients’ expectations are now perfectly clear and precise: they want aesthetic and functional results thanks to aesthetic appliances.Current advantages in using a combination of lingual and buccal appliances have now made it possible to perform ideal global predictable treatment, giving a stable and functional bite in a harmonious and balanced face. I have quite naturally drawn from the benefits of each system, namely the ability to apply with success a mix of those appliances to my patients (adults or adolescents).
This aim of this article is to show how to easily manage this form of ‘Combination case’ even in the context of multidisciplinary treatment, where the orthodontist is naturally called on to occupy a central role amid a galaxy of specialists.
Anamnesis
A 56-year-old female patient presenting a severe open bite and a narrow maxilla complaining of daytime somnolence, mood changes (increased irritability), headaches and problems of concentration. Before creating a treatment plan, I referred the patient to an ENT specialist for precise diagnosis of OSAHS). The patient underwent ear, nose and throat assessments including auditory and respiratory tests, a daytime sleepiness questionnaire, polysomnography and radiologic investigations.She was referred to a maxillofacial surgeon, in order to prioritize the problems as well as the solutions necessary for the orthodontic treatment plan.
Diagnosis
Figures 1A-D, Figures 1E-I, Figures 1J-N, Figure 10The patient had skeletal Class III tendency, skeletal and dental open bite, class I, class III dental relationship with complete open bite from 17 to 27. With constrictive maxilla the midlines were not coincident and the functional problems made the diagnosis worse.
The dental panorex confirmed a good level of bone, no periodontal problem, absence of 38, 37, 48, extrusion of 18, 28, a ceramic crown and root filing of 26 and amalgam crown filling on posterior teeth. The TMJ were also seen to be satisfactory.
The side view film with the initial cephalometric analysis confirmed the skeletal Class III and open bite discrepancies, the deficit of the upper jaw head development and a slight incisor’s proclination in relation with the tongue posture. (Table 1)
The functional assessment showed that the patient suffered a Preoperative Apnea Hypopnea Index (AHI) severity of 30 per hour. The maxillary nasal constriction might increase nasal resistance and alter the tongue posture leading to narrowing of the retroglossal airway.
-
Treatment Plan
The surgeon recommended two-step maxillo-mandibular surgery with a first line transverse procedure and a double Maxilla Mandibular Advancement (MMA).- The first line transverse procedure is used to forestall relapse of the transverse dimension. According to Chamberlan et al. (3) transverse relapse occurs for 30% in the molar segment whatever mode of surgical expansion is used.
- The double Maxilla Mandibular Advancement (MMA) is acknowledged to be the most effective treatment for OSA in adults as it protracts the pharyngeal tissues connected to the maxilla and the hyoglossal complex connected to the mandible. (2)
Diagnosis, biomechanical reasons, functional considerations and surgeon’s recommendations were used to design a treatment plan incorporating a ‘combo case’ approach with upper 3M™ Incognito™ Appliance and lower 3M™ Clarity™ Advanced Ceramic Brackets.
Phase I: Early Orthodontic Treatment
Surgical assisted disjunction with 3D digital expander. See Figures 2A-C, Figures 2D-E.The 3D expander was bonded one day before surgery.
The expander was left in place for 4 months, and a retention tray (Colgate® Oral Care, Essix Retainer) was used to maintain the results and worn night and day during the Incognito Appliance System manufacture.
Radiographs were taken before the second phase, showing a huge maxillary expansion of the palatal suture with a good root integrity, a maxillary advancement of point A in relation to SN (SNA=4,7°) but an aggravation of the skeletal open bite (Go-Gn/SN=37,5°) and occlusal plane to SN (17,5°). (Table 2)
After the disjunction phase, the treatment needed to be supported by pre-and post-operative maxillofacial physiotherapy to reinforce the automatic tongue reflex.
Phase II: Pre-Surgical Esthetic Bracket Application
The pre-surgical preparation included a combination of Incognito Brackets and Clarity Advanced Brackets followed by bi-Maxillary surgery. See Figures 3A-E, Figure 3F, Figures 3G-K, Figures 3L-P, Figures 3Q-U, Table 3During the second phase, the maxillary distraction facilitated orthodontic alignment and transverse coordination without giving rise to major facial changes. Progressively, wire after wire, the bite closed, and there was a spectacular improvement in her breathing pattern with an improved position of the tongue. Her newly-found anatomic equilibrium achieved in the first surgery, stabilized her ventilator function and her swallowing. The shift from oral to nasal breathing was confirmed by the ENT specialist.
The second phase of surgery was not performed as the patient was more concerned by function than esthetics and was happy with the results. She could breathe normally, close the bite and obtain competent lips.
Phase III: Final Inter-Digitation of the Dental Arches. Finishing.
During finishing (0182x0182 Beta III Titanium) the patient wore Inter-maxillary elastics. See Figure 4A-E
Phase IV: Retention and Stabilization
Figure 5A-D, Figure 5E-I, Figure 5J
The final cephalometric analysis and the structural superimpositions show an incredible anterior mandibular auto-rotation with a counter clockwise movement of the face, the mandibular plane and the occlusal plane leading to a skeletal and bite closure.
Patricia Obach-Dejean, DDS, Orthodontic Spec., Clinical Advisor Western Europe
-

Dr Obach-Dejean did her dental training at Toulouse University and obtained her specialization in Orthodontics diploma at Paris V University. Since 1987, she has been in specialist practice in Auch 32000 ( South West of France). 2011-2015 she taught Postgraduate students in Orthodontics at Toulouse University.
She is French Board (BFO) and European Board (EBO) certified. She is Past President of the European College of Orthodontics (CEO), Past President of the French Federation of Othodontics ( FFO).
And she is very much involved in the European orthodontic societies: She is past Director of the European Board examiners and Past Chairman of the Scientific Committee of the Angle society of Europe (ASE) and Active Member since 2001.
She is a clinical instructor in Lingual Orthodontics and a Clinical Advisor for the Western Europe Incognito™ Lingual Appliance System since 2016.
-
Receive Innova via Email
Don't miss an issue! Subscribe to receive Innova via email as soon as it becomes available.
Thank You For Signing Up
Thank you for your subscription! Innova is a relevant and educational source for orthodontic solutions and treatment options from 3M Oral Care.
Please check your email for the most current issue of Innova.
Our Apologies...
An error has occurred while submitting. Please try again.
